Healthcare politics shapes every layer of the health system, from boardroom strategies and regulatory decisions to the everyday experiences of patients and families who rely on timely care. In this arena, health policy debates drive the framework for access, quality, and cost, influencing how services are funded, delivered, and prioritized across clinics, hospitals, and communities. Understanding how healthcare legislation translates into real-world changes helps patients, providers, and policymakers align incentives toward improved care, better coordination, and tangible, measurable improvements in health outcomes. For readers seeking practical insight, this introduction connects policy discussions to everyday care, highlighting reform trajectories, coverage shifts, and the practical timelines through which reforms take effect in clinics and communities, including how providers, patients, and payers adapt to new rules. By examining the links among debates, lawmaking, and the lived experience of care, we can see why this topic matters to everyone involved in health, from clinicians and administrators to patients and caregivers, and why informed participation matters for better care and sustainable systems.
Beyond the surface debates, the health policy landscape is really about how systems organize, fund, and monitor care across diverse populations. Terms such as care delivery policies, reimbursement reforms, and governance of health services describe the mechanisms behind meaningful change. By looking at payer strategies, provider networks, and community health initiatives, we can infer how shifts in policy shape day-to-day practice. This framing emphasizes care quality, access, and equity as outcomes of how reforms are designed and implemented. In short, the conversation moves from abstract ideals to concrete changes in how health services are organized and delivered.
Healthcare politics and patient outcomes: how debates shape access, quality, and care
Healthcare politics shapes who gains timely access to care, how providers organize services, and the health outcomes families experience. In this arena, debates among lawmakers, payers, providers, and patients crystallize around coverage, subsidies, and reimbursement structures. When the public engages with health policy debates, they are hearing about the levers that widen access or create barriers. The influence of policy on care is visible in essential health benefits, preventive services, and the availability of primary care in rural or underserved communities. Therefore, the political process is not abstract; it directly touches patient outcomes through access and affordability.
Policy impacts on care emerge through the language of healthcare legislation. Laws translate political goals into funded programs, rules for provider payment, and performance incentives that shape everyday practice. As debates emphasize value, quality, and equity, legislation seeks to align incentives toward better patient outcomes, more efficient care, and fewer avoidable hospitalizations. Yet the real-world effect depends on careful implementation, provider adoption, and transparent measurement of results.
Beyond Capitol Hill, the interplay of debates and legislation influences the patient journey. When health policy reform expands coverage and reduces cost-sharing, individuals are more likely to seek preventive care and adhere to treatment regimens. Conversely, restrictive measures can create gaps in care, delays in treatment, and widening disparities. Understanding healthcare politics through the lens of patient outcomes helps patients, clinicians, and advocates anticipate changes, ask informed questions, and participate in reforms that prioritize care quality and value.
From health policy debates to care delivery: translating healthcare legislation into health policy reform and patient outcomes
From health policy debates to actual care delivery, the path begins with the legislative process. Proposals move through committees, hearings, and votes, guided by evidence on costs, benefits, and implementation challenges. Public input and advocacy often tilt the balance, shaping which provisions survive into healthcare legislation. In this space, the core question is how policy reform will impact care access, affordability, and quality in practice, and how those changes will be measured by patient outcomes.
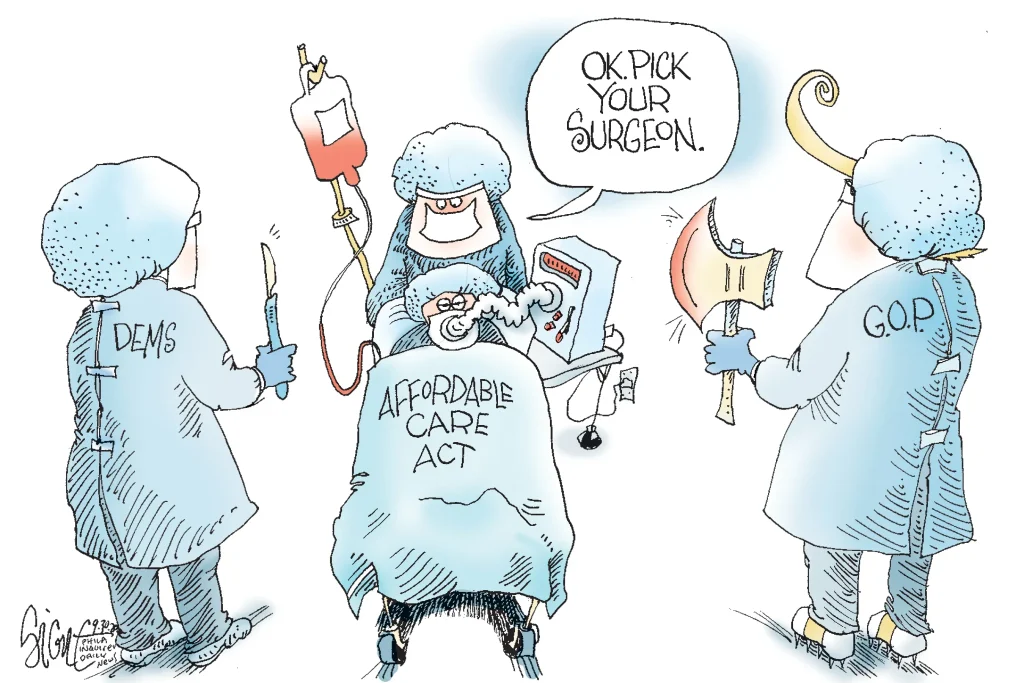
Healthcare legislation crafted through intense health policy debates often serves as a blueprint for health policy reform. The Affordable Care Act is a historical touchstone illustrating how debates translate into law, expand coverage, and reform payment models. The resulting policy changes—subsidies, essential health benefits, and incentives for coordinated care—demonstrate how policy impacts on care can drive tangible improvements in patient outcomes, while also prompting ongoing adjustments and refinements in health policy reform.
Looking forward, accountability and transparency are essential as health policy debates continue to shape care delivery. Stakeholders will watch how policy decisions affect access, prevention, and outcomes, with a focus on reducing disparities and improving value. As healthcare legislation evolves, health policy reform will likely emphasize data-driven improvements, patient-centered delivery, and scalable models of care coordination that translate debates into better patient outcomes and sustained improvements in the health system.
Frequently Asked Questions
In healthcare politics, how do health policy debates influence healthcare legislation and patient outcomes?
Health policy debates help set priorities, frame proposed solutions, and shape the language of healthcare legislation. The resulting laws determine funding, coverage, and delivery rules that directly affect patient outcomes by expanding access, improving coordination, and controlling costs. The magnitude of policy impacts on care depends on how effectively reforms are implemented and monitored.
What is the role of stakeholders in health policy reform within healthcare politics, and how do these efforts translate into policy impacts on care and patient outcomes?
Stakeholders—lawmakers, regulators, payers, providers, and patients—contribute evidence, advocacy, and practical insights that inform health policy reform. Their involvement helps ensure reforms are feasible, properly financed, and aligned with real-world care delivery. When reforms are well-designed, they influence care delivery, access to services, and ultimately patient outcomes, reflecting the policy impacts on care.
| Topic | Core Idea | Impact on Care and Outcomes |
|---|---|---|
| Introduction | Healthcare politics is the arena where policy ideas, public sentiment, and practical realities collide, shaping access, quality, and costs for real people. | Understanding this helps patients navigate the system, assist providers in delivering better care, and guide policymakers to craft legislation that improves health outcomes. |
| The landscape: Players and Power | An ecosystem of key actors—lawmakers/regulators, payers, providers, and patients/families—each with distinct priorities and constraints. They shape how care is financed and delivered. | Their interactions determine policy direction, implementation, and day‑to‑day care experiences. |
| Debates shaping policy: Core tensions | Core tensions include: access vs affordability; quality/innovation vs price controls; centralized standards vs local flexibility; public vs private options. | These tensions influence policy design and, ultimately, patient outcomes. |
| The legislative process: From proposal to policy | Policies originate in the executive, committees, or bipartisan groups and progress through hearings, amendments, and votes; public opinion and advocacy shape the direction. | A bill’s passage and framing affect how it is implemented and its impact on patients and providers. |
| Historical touchstone: ACA as reference | ACA aimed to expand access, improve quality, and reduce costs via subsidies, benefits, and new delivery incentives. | Shows how debates translate into law and influence real-world patient outcomes. |
| Impact on patient outcomes | Policy choices affect coverage, access, and payment reforms that incentivize care coordination and outcomes. | Expanded coverage and value-based care can improve chronic disease management and reduce unnecessary hospitalizations. |
| Case studies and practical implications | State reforms, telehealth pilots, reimbursement shifts, and preventive care incentives demonstrate policy tools at work. | Real-world changes in provider behavior and patient access illustrate potential health gains or barriers. |
| Public engagement and accountability | Evidence, stakeholder input, and transparent evaluation underpin credible policy. Public participation ensures responsive policies. | Policies that reflect patient voices tend to produce better alignment with community needs and outcomes. |
| Future directions | Trends include telehealth, precision medicine, and value-based care, plus a focus on social determinants and data-driven reform. | These directions will shape the trajectory of health policy and patient outcomes. |
Summary
Conclusion